At the start of 2026, the healthcare industry is entering a decisive phase. The integration of biology, physics and data science is giving rise to a major new discipline: bioconvergence. For decision-makers, this shift marks the end of silo-based innovation and the emergence of medicine driven by the complex organization of living organisms.
The continuum: from cellular data to tissue architecture
Clinical value no longer lies in the study of the isolated cell, but in its ability to interact with its micro-environment. This transition from unit to tissue is the new foundation of precision medicine.
Ariah embodies this transition through space biology. Ariah integrates biology, advanced cellular imaging techniques and develops its own software tools that use AI to map interactions at the heart of tissues. It identifies transcriptomic signatures invisible to conventional methods. This understanding of the cellular scale in a real-life context enables us to anticipate treatments and their effects with unrivalled precision.
At the same time, Therapixel has proven that AI can interpret micro-changes in tissue organization with greater reliability than the human eye. This mastery of data reduces uncertainty and optimizes refund strategies with insurers.
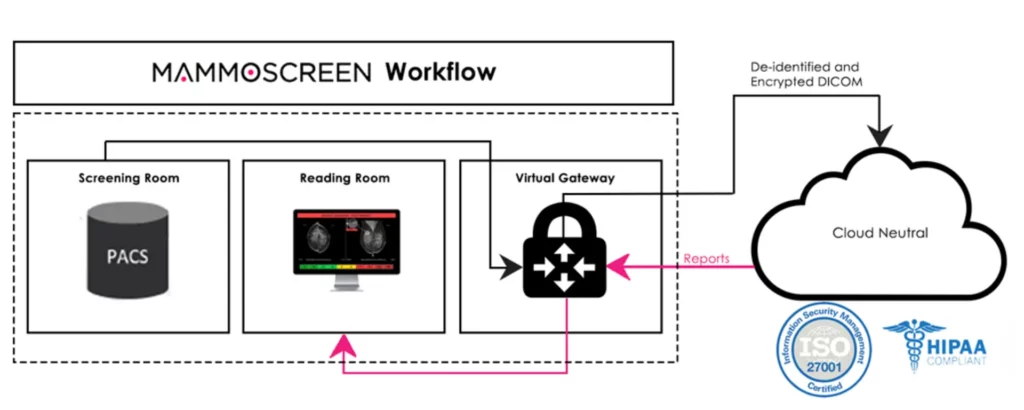
Bioconvergence between medical data and artificial intelligence to optimize clinical analysis workflows and diagnostic reliability. © Therapixel
Ex vivo validation: securing the value chain
The critical cost of failures in the clinical phase is met by the creation of functional human models. In 2026, early human data has become the regulatory gold standard, propelled by Environmental, Social and Governance (ESG) requirements and the end of systematic animal testing.
This is where Exadex-Innov‘s solutions come in. Working on human adipose tissue models kept alive, the platform enables molecules to be tested on a reactive tissue structure. This validation stage secures laboratories’ financial assets by eliminating toxic or ineffective candidates before the massive investment required for human trials.
Production and sovereignty: the infrastructure of precision
Artificial intelligence and physics are transforming pathology into a performance industry. Beyond diagnostics, it’s the production tool that’s being relocated:
Sound biofabrication: MimiX uses ultrasound waves to manipulate cells and recreate complex tissues in a matter of seconds, a major advance in wound care.
Thanks to bioconvergence, sound biofabrication opens up new prospects for tissue regeneration and precision medicine. © MimiX
Macro impact: ESG and health economy
The adoption of bioconvergence responds to a triple imperative. Firstly, profitability, by reducing the R&D cycle. Secondly, sustainability, by minimizing the use of biological and animal resources. Finally, a public health imperative: by treating better and faster, we reduce the burden on health insurance systems.
Conclusion: Towards a new era of therapeutic sovereignty
Bioconvergence is no longer just a laboratory promise; in 2026, it has become the backbone of a rapidly changing healthcare industry. By breaking down the boundaries between disciplines, actors such as Ariah, Exadex-Innov and MimiX are not just improving healthcare: they are redefining the sector’s economic and ethical value.
For decision-makers, this paradigm shift calls for a new agility. Investment is no longer measured solely in terms of the molecule, but in terms of the ability to integrate cross-disciplinary technologies, from AI to acoustic physics, to master the complexity of the living world. At the crossroads of clinical performance and ESG commitment, bioconvergence is emerging as the essential lever for building a more human, more precise and, finally, sustainable medicine.